
Female Incontinence |
||
The blader is the name for a structure in the body that stores urine, which is made by the kidneys. Simply speaking, the bladder is a bag that expands as it fills with urine and contracts when it is full to empty. The middle part of the wall of the bladder is a muscle that can contract urine out from the bladder - this muscle is called the detrusor muscle. The bladder has an inner lining known as 'urothelium'. In women, urine is passed from the bladder to the outside world through the urethra. In men, the prostate sits between the bladder and the urethra, and the urethra is much longer in men than in women. What is urinary incontinence?
Urinary incontinence is the inability to control urination. This can occur temporarily if there is a short-term problem such as a urinary infection and this can usually be resolved promptly. Longer term (more than 3 months) often indicate an underlying problem. Stress urinary incontinence is the name for incontinence most commonly due to lack of support for the bladder structures. Symptoms aren't reliable in making a diagnosis for the absolute cause for urinary leakage, but can give an indication. If you leak most often with physical activity (e.g. coughing, sneezing, lifting or exercise), then stress incontinence is likely to be present. If you leak when you have a strong desire to empty your bladder, but can't reach the toilet fast enough, then urge incontinence is present. Urge incontinence may be due to the bladder muscle contracting when you don't want it to do so ('detrusor instability'). Sometimes, both stress and urge incontinence can exist together, and this is known as mixed incontinence Why talk about bladder control?
Women, and some men, have bladder control problems. it is a very common problem affecting women of all ages. In young women, urine leakage can occur after giving birth to a child.
Sometimes it occurs after periods stop (menopause) or in older women in their 70s. Incontinence is not something to be ashamed and affects many women. Urine leakage is not normal and can be successfully treated in the majority of women. Why do I leak when I cough, exercise, laugh or sneeze?
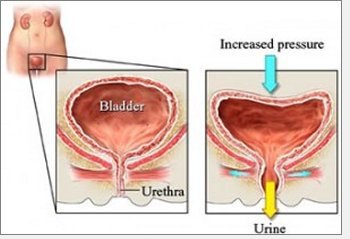
Activities such as these increase the pressure on the bladder literally forcing urine out of the bladder. Usually, the muscles in the pelvis support the bladder and urethra (water pipe) prevent urine from coming out. These muscles can be weakened by pregnancy, obesity, menopause or an inherited tissue weakness. This is usually known as 'genuine stress incontinence'.
Sometimes, the problem is due to a weakness in the wall of the urethra (water pipe) rather than the bladder or urethral support. Less commonly, coughing, exercise, laughing or sneezing can stimulate the bladder muscle to contract and that causes urine to leak. This is known as Valsalva induced detrusor overactivity. Why do I need to rush to the toilet when I feel the need to pass urine?
Normally, the bladder muscle should contract only when you pass urine. Sometimes, the bladder muscle contracts before it is full and when you would rather not go to the toilet. If you don't reach the toilet on time, you might leak.
During the day and night, the urge to pass urine may be overwhelming and so you go to the toilet more than other people. If you don't make it to the toilet on time, incontinence may occur. If the bladder muscle itself is contracting inappropriately, this condition is often known as 'detrusor overactivity'. Sometimes, there are important causes for this problem, but often no specific cause is found. How does bladder control normally occur?
The bladder is like an expandable bag that holds urine as it fills. When the bladder is full, the pelvic floor relaxes, the bladder muscle ('detrusor') contracts and urine is passed. Urine passes from the bladder through a tube called the urethra (water pipe) to the outside world. Usually, the desire to pass urine occurs when the bladder is almost completely full, but in some people, the bladder muscle (detrusor) contracts far too early. This gives rise to an urgent desire to pass urine that can sometimes be too strong to stop resulting in a leak. This is often called detrusor overactivity. Thus, normal bladder filling occurs with the detrusor (bladder muscle) remaining relaxed and not overactive.
As the bladder becomes full, coughing, lifting and other activities do not usually cause urine leakage because the urethra (water pipe) is supported. The support comes from the pelvic floor, which is a layer of muscle under the bladder. Lack of urethral support results in urine leakage with stressful activities. Urethral support can be improved by pelvic floor exercises, losing weight, drugs and new procedures that can be performed as day cases or with an overnight stay.
For bladder control to be effective, the nervous system has to be working normally. How do you work out why bladder control is poor and urine leakage occurs.
In the majority of women, the cause is principally either of the two problems listed above ie stress incontinence or detrusor overactivity. It can be difficult to distinguish between the two from symptoms alone, as they can often overlap in 3 in 10 cases.
Symptoms that suggest that detrusor overactivity is present include the sudden urge to pass urine (urgency) that occurs day and night, together with urine leakage that occurs with urgency ('urge incontinence'). Urine is passed frequently and often in large amounts when the strong urge is present.
Stress incontinence usually occurs with activity and the leakage is usually only a few drops only. Urine leakage rarely occurs at night except in the worst cases. Symptoms and the findings on physical examination can help sometimes. The 'cough test' determines whether leakage occurs on coughing or not. However, often it is difficult to reliably rule out one or other condition. If the symptoms do not resolve after simple help, additional tests are required. These include
• Urodynamics (pressure/flow studies): This is a test in which a narrow tube is placed in the bladder and rectum ('backpassage') so that the pressure in each can be recorded. What can I do myself to reduce urine leakage? There are simple things one can do: pelvic floor exercise and lose weight.
It is helpful if you can complete a questionnaire on the severity of urinary incontinence as this helps doctors to make decisions on the need for investigations or treatment. The following Adobe PDFs can be downloaded and printed: Can pelvic floor exercises and physiotherapy help?
Providing the exercises are done, they will help, and they will need to be done for the rest of one's life. They can be performed by oneself or taught with the aid of a physiotherapist. Please see Pelvic Floor Exercises.
They help urinary leakage that occurs due to stress incontinence as well as due to detrusor overactivity (urge incontinence).
There are additional aids that one can use to improve the efficacy of pelvic floor exercises. These include biofeedback machines. Again, these have to be performed regularly like any exercise programme.
Why exercise pelvic muscles?
Life's events can weaken pelvic muscles. Pregnancy, childbirth, and being overweight can do it. Luckily, when these muscles get weak, you can help make them strong again.
Pelvic fitness in minutes a day
Exercising your pelvic floor muscles for just 5 minutes, three times a day can make a big difference to your bladder control. Exercise strengthens muscles that hold the bladder and many other organs in place. How do you exercise your pelvic muscles?
Find the right muscles.
Female Pelvic Anatomy You should tighten the two major muscles that stretch across your pelvic floor. They are the "hammock" muscle and the "triangle" muscle. Here are three methods to check for the correct muscles. Try to stop the flow of urine when you are sitting on the toilet. If you can do it, you are using the right muscles. Imagine that you are trying to stop passing gas. Squeeze the muscles you would use. If you sense a "pulling" feeling, those are the right muscles for pelvic exercises. Lie down and put your finger inside your vagina. Squeeze as if you were trying to stop urine from coming out. If you feel tightness on your finger, you are squeezing the right pelvic muscle. Don't squeeze other muscles at the same time.
Be careful not to tighten your stomach, legs, or other muscles. Squeezing the wrong muscles can put more pressure on your bladder control muscles. Just squeeze the pelvic muscle. Don't hold your breath.
Do your pelvic exercises at least three times a day.
Every day, use three positions: lying down, sitting, and standing. You can exercise while lying on the floor, sitting at a desk, or standing in the kitchen. Using all three positions makes the muscles strongest. Image of the bladder, and the related muscles used in the urination process.
Female Bladder
Points to remember
• Weak pelvic muscles often cause bladder control problems. Can drugs or medicines help?
For women with stress incontinence, Yentreve or duloxetine is a new drug that helps women by reducing the number of times incontinence occurs. It is not a complete cure, but does make some women better and maybe usefully combined with pelvic floor exercises. The feeling of nausea may occur, but usually ameliorates after the first few weeks. This drug should only be taken on the advice of a doctor who knows your medical history well.
For women with urge incontinence or detrusor overactivity, drugs such as Detrusitol (tolterodine), Lyrinel (oxybutynin), Regurin (trospium), propiverine, or solifenacin may help. To some extent these can give rise to a dry mouth or constipation. These medications should be combined with changes in drinking habits such as reducing caffeine and alcohol consumption. What is a Urodynamic Test
This is the name for a test performed as an outpatient to determine how the bladder works. It takes about one hour to do. The aim is to understand the activity of the bladder whilst it is filling with urine and during activity. To do this, a very narrow tube has to be passed into the bladder through the urethra.
Why am I having this test?
Female Urodynamic Testing
It can also help predict whether drugs or surgery are likely to have a good result for; • Stress incontinence in women What should I do before this test?
It is not necessary to fast the night before or take laxatives. As long as the urine test is normal, the study is very safe and can be performed with minimal discomfort. It is important to arrive with a full bladder since it may be necessary to pass urine into a special machine ("urinary flow rate test") before the formal urodynamic test and for a test by the nurse to determine if an infection is present. Usually, a nurse and an x-ray technician will be in the room during the test.
What will happen during the test?
You will need to undress and put on a gown. Local anaesthetic jelly will be placed in the urethra (the water-pipe from the bladder). A narrow tube (catheter) will be placed by a doctor or nurse through the urethra ('water pipe') into the urinary bladder. In addition, another narrow tube will be placed in the rectum (the 'back passage'). The study can be performed standing or sitting. A computer will record all of the measurements and produce a record of the events during the test.
What happens after the test?
Half an hour after the test, you will be able to go home. You may experience some burning when passing urine for a few days and this is normal. There may be some blood in the urine, but as long as large clots are not formed, the bleeding will settle if you drink plenty of fluid. You can resume regular diet, medications, and normal activity levels after you leave.
|
|
|
Summary |
|
