Interstitial Cystitis |
||
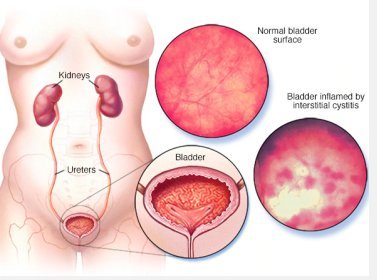
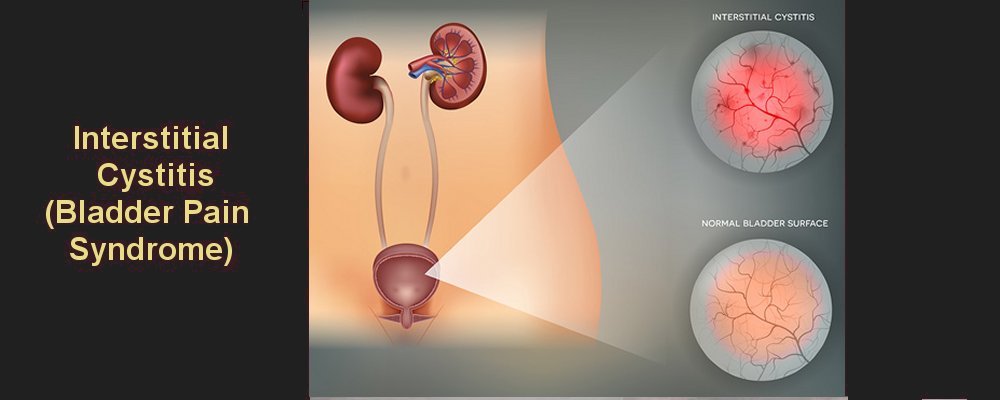
Interstitial cystitis (IC)/bladder pain syndrome (BPS) is a chronic bladder health issue. It is a feeling of pain and pressure in the bladder area. Along with this pain are lower urinary tract symptoms which have lasted for more than 6 weeks, without having an infection or other clear causes.
Symptoms range from mild to severe. For some patients the symptoms may come and go, and for others they don't go away. IC/BPS is not an infection, but it may feel like a bladder infection. Women with IC/BPS may feel pain when having sex. The more severe cases of IC/BPS can affect your life and your loved ones. Some people with IC/BPS have other health issues such as irritable bowel syndrome, fibromyalgia, and other pain syndromes.
The bladder and kidneys are part of the urinary system, the organs in our bodies that make, store, and pass urine. You have 2 kidneys that make urine. Then urine is stored in the bladder. The muscles in the lower part of your abdomen hold your bladder in place.
What are the symptoms of of interstitial cystitis/ bladder pain syndrome? PainThe symptoms of IC/BPS vary for each patient, but the most common sign is pain (often with pressure). Patients with IC/BPS may have bladder pain that gets worse as the bladder fills. Some patients feel pain in other areas in addition to the bladder, such as the urethra, lower abdomen, lower back, or the pelvic or perineal area (in women, behind the vagina and in men, behind the scrotum). Women may feel pain in the vulva or the vagina, and men may feel the pain in the scrotum, testicle, or penis. The pain may be constant or may come and go.
FrequencyIC/BPS sometimes starts with urinary frequency. Frequency is the need to pass urine more often than normal. The average person urinates no more than 7 times a day. He or she does not have to get up at night more than once to use the bathroom. A patient with IC/BPS often has to urinate frequently both day and night. As frequency becomes more severe, it leads to urgency.
UrgencyUrgency to urinate is a common IC/BPS symptom. Some patients feel an urge that never goes away, even right after voiding. A patient may not notice or see this as a problem. In other cases, the onset is much more dramatic, with severe symptoms occurring within days, weeks or months. Many patients with IC/BPS can point to certain things that make their symptoms worse. For some, their symptoms are made worse by certain foods or drinks. Many patients find that symptoms are worse if they are under stress (either physical or mental).
For women, the symptoms may vary with their period. Both men and women with IC/BPS can have sexual problems due to this health issue. Women may have pain during sex because the bladder is right in front of the vagina. Men may have painful orgasm or pain the next day. It is unusual to experience leaking of urine with this disorder, and urinary leaking might be a sign of another problem.
Who gets the symptoms of interstitial cystitis/ bladder pain syndrome?
Because there is no standard technique to diagnose IC/BPS, it is often hard to estimate the number of people affected. IC/BPS is typically 2 to 3 times more in common in women than in men, and data have shown the risk of IC/BPS increases with age.
The difference between men and women may not really be as high as we think, because some men diagnosed with "prostatitis" (swelling of the gland that makes semen in men) or similar conditions with different labels may really have IC/BPS. At this time, there is no evidence that stress causes IC/BPS in the first place. However, it is well-known that if a person has IC, physical or mental stress can make the symptoms worse.
How interstitial cystitis/ bladder pain syndrome can affect your life?
IC/BPS can get in the way of your social life, exercise and sleep, and can cause a great deal of distress. Without treatment, IC/BPS symptoms make it hard to get through your day or even be able to work. IC/BPS may affect your relationship with your spouse and family. It can also rob you of a good night's sleep. Too little sleep will leave you tired and unhappy.
What causes interstitial cystitis/ bladder pain syndrome?
Experts do not know exactly what causes IC/BPS, but there are many theories, such as:
Non specific behaviours (such as smoking) are known to increase your risk of IC. Having a family member with IC/BPS may increase your risk of getting IC/BPS. Patients with IC/BPS may have a substance in the urine that inhibits the growth of cells in the bladder tissue. So, some people may be more likely to get IC/BPS after an injury to the bladder, such as an infection.
How is interstitial cystitis/ bladder pain syndrome diagnosed?
At this time, there is no medical test that can say a person has IC/BPS. Also, there is no test to say a person does not have IC/BPS. To make a diagnosis, your doctor will first decide whether the symptoms are typical of IC/BPS. Next, they need to rule out other health issues that might be causing the symptoms. Some believe that IC/BPS is present if a patient has symptoms and no other cause for those symptoms is found. Others believe that more tests are needed to find out whether the patient has IC/BPS.
Below are some ways your health care provider may find out if you have IC/BPS : Medical HistoryYour doctor will ask you a number of questions about:
Physical and Neurological ExamYour doctor will examine you to look for the cause of your symptoms. In women, the physical exam will likely include your abdomen, the organs in your pelvis, and your rectum. In men, a physical exam will include your abdomen, prostate, and rectum. Your doctor may also do a neurological exam to rule out any other problems. Patients with IC/BPS may have other mental health and/or anxiety disorders which may be linked to their condition.
Baseline Pain and Voiding TestsSince the hallmark sign of IC/BPS is pain, your health care provider will conduct tests and ask you to fill out a series of questionnaires to find out your baseline pain value. The goal of the evaluation is to find pain location(s), intensity, and characteristics, and to identify factors that make pain or discomfort better or worse. Your doctor will also ask how often you void. A very low voiding frequency or high voided volume should prompt your health care provider to look for some other urological condition beside IC/BPS.
Other TestsYour doctor may run other tests to rule out health issues that may seem like IC/BPS. These include:
Urodynamic evaluation: This involves filling the bladder with water through a small catheter (tube to drain fluid from the body). This measures bladder pressures as the bladder fills and empties. In patients with IC/BPS the bladder has a small capacity and perhaps pain with filling.
Cystoscopy: Using a special tool, your doctor looks inside the bladder. This test can rule out other problems such as cancer. The doctor can see actual ulcers through the cystoscope in some patients with IC/BPS. If a person has symptoms of IC/BPS and cystoscopy shows ulcers, the diagnosis is fairly certain. If bladder stones, tumours or ulcers are seen during cystoscopy, the doctor can take care of them at the same time as the bladder biopsy, which is used to rule out other bladder diseases.
At this time, there is no clear answer about the best way to diagnose IC/BPS. However, if a patient has typical symptoms and a negative urine exam showing no infection or blood, then IC/BPS should be suspected.
What is the treatment for interstitial cystitis/chronic bladder pain syndrome?
No single treatment works for all people with IC/BPS. Treatment must be chosen for each patient based on symptoms. Patients usually try different treatments (or combinations of treatments) until good symptom relief occurs.
It is important to know that none of these IC/BPS treatments works right away. It usually takes weeks to months before symptoms improve.
Even with successful treatment, the condition may not be cured. It is simply in remission. But, most patients can get significant relief of their symptoms and lead a normal life with treatment.
Most treatments are aimed at symptom control. IC/BPS treatment is often done in phases with constant monitoring of your pain and quality of life. It is important to talk to your health care provider about how your treatments are working so that together you can find the best treatment option for you.
The following are the different lines of IC/BPS treatment:
First Line: Lifestyle Changes
Lifestyle changes, are often the first treatments used to manage IC/BPS. In behavioural therapy, you make some changes in the way you live day-to-day. This may include changing your diet, or practicing methods that may help control your symptoms. Most patients don't get rid of all their symptoms with lifestyle changes. But many do have fewer symptoms using these types of treatments.
Manipulative Physical TherapyPatients with IC/BPS often have tenderness and/or pain in the pelvic floor area, and sometime manipulative physical therapy can reduce symptoms. There is evidence that physical therapy exercises to strengthen the pelvic floor muscles do not improve symptoms, and often make them worse, so activities such as Kegel exercises are not recommended for patients with IC/BPS.
Limiting StressEmotional and mental stress can worsen IC/BPS symptoms. Patients are encouraged to come up with coping methods to deal with family, work and/or past painful experiences, and may need to seek additional help to develop the best coping strategies to help manage their pain.
Limiting Certain Foods and DrinksMost (but not all) people with IC/BPS find that certain foods make their symptoms worse.
There are 4 foods that patients most often find irritating to their bladder:
Other foods that bother the bladder in many patients are:
Elimination DietThe list of foods that have been said to affect IC/BPS is quite long, but not all foods affect all patients the same way. Each patient must find out how foods affect his or her own bladder. The simplest way to find out whether any foods bother your bladder is to try an "elimination diet" for 1 to 2 weeks. On an elimination diet, you stop eating all of the foods that could irritate your bladder. IC/BPS food lists are available from many sources and a good one is the IC Smart Diet which you can download here.
If your bladder symptoms improve while you are on the elimination diet, this means that at least 1 of the foods was irritating your bladder.
The next step is to find out exactly which foods cause bladder problems for you. After 1 to 2 weeks on the elimination diet, try eating 1 food from the IC/BPS food list. If this food does not bother your bladder within 24 hours, this food is likely safe and can be added back into your regular diet.
The next day, try eating a second food from the list, and so on.
In this way, you will add the foods back into your diet one at a time, and your bladder symptoms will tell you if any food causes problems for you. Be sure to add only 1 new food to your diet each day. If you eat a banana, strawberries and tomatoes all in the same day, and the IC/BPS symptoms are worse that evening, you will not know which of the 3 foods caused the symptoms to flare up.
Second Line - Medication
When lifestyle changes do not help enough, your health care provider may ask you to try a prescription drug. You may take the drug alone or along with behavioural therapy. The 2 types of prescription drugs that may be recommended are, oral and intravesical drugs. There are many types of oral drugs, and the side effects range from drowsiness to upset stomach. Intravesical prescription drugs are placed directly into the bladder with a catheter.
Oral Pentosan Polysulfate No one knows exactly how this drug works for IC. Many people think that it builds and restores the protective coating of the bladder tissue. It may also help by decreasing swelling or by other actions. Possible side effects are not common, but may include nausea, diarrhoea and gastric distress. A small percentage of people may have temporary hair loss. It often takes at least 3 to 6 months of treatment with this drug before you notice improvement in symptoms. It is effective in relieving pain in about 30 out of every 100 patients.
Dimethyl Sulfoxide (DMSO)Dimethyl sulfoxide (DMSO) is placed into the bladder through a catheter. This is usually done once a week for 6 weeks. Some people keep using it now and then as maintenance therapy. No one knows exactly how DMSO helps interstitial cystitis. It may block swelling, decrease pain sensation and remove a type of toxin called "free radicals" that can damage tissue. Some health care providers combine DMSO with other drugs such as heparin or steroids (to decrease inflammation). No studies have tested whether these combinations work better than dimethyl sulfoxide alone. The main side effect is a garlic-like odor that lasts for several hours after using DMSO. For some patients, DMSO can be painful to place into the bladder, but the pain can often be relieved with a local anaesthetic.
HydroxyzineHydroxyzine is an antihistamine. It is thought that some patients with IC/BPS have too much histamine in the bladder that leads to pain and other symptoms. An antihistamine may be helpful in treating IC/BPS. The main side effect is drowsiness. However, this may be a benefit because it helps the patient to sleep better at night and get up to pass urine less frequently. The only antihistamines that have been specifically studied for IC/BPS are hydroxyzine and (more recently) cimetidine. It is not known whether other antihistamines also help treat IC/BPS.
AmitriptylineAmitriptyline is described as an antidepressant, but it actually has many effects that may improve IC/BPS. It has antihistamine effects, decreases bladder spasms, and slows the nerves that carry pain messages. Amitriptyline is widely used for other types of chronic pain such as cancer and nerve damage. The most common side effects are drowsiness, constipation and increased appetite.
HeparinHeparin is similar to pentosan polysulfate and probably helps the bladder by similar mechanisms. Heparin must be placed into the bladder with a catheter. The usual dose is 10,000 to 20,000 units daily or 3 times a week. Complications are rare because the heparin stays in the bladder only and does not usually affect the rest of the body.
Third Line: Neuromodulation, Cauterization and Injections
Neuromodulation TherapyIf lifestyle changes and prescription drugs don't work, or pain or side effects interfere with your quality of life, more advanced therapies may be a better choice. You will most likely be referred to a specialist who treats patients with IC/BPS, such as a urologist. After reviewing your treatment history, the specialist may suggest neuromodulation therapy. Neuromodulation therapy is the name given to a group of treatments that deliver harmless electrical impulses to nerves to change how they work.
Bladder Ulcer CauterizationIf you have a bladder ulcer, having it cauterized under anaesthesia or having steroid injections may give long-term relief for up to a year or more. This treatment can be repeated if necessary.
InjectionsSome injections of Botox® can be given if other treatments have not provided adequate symptom control and there is no improvement in quality of life. Small doses of this drug can paralyze muscles. When injected into the bladder muscle, it may help with the pain of IC/CBPS. This treatment can wear off, and you may need to have another treatment 6 to 9 months after the first injection. Your health care provider should follow you closely to watch for complications, including difficulty in passing urine. Fourth Line: Cyclosporine
When other treatments have not been successful, cyclosporine can be used. You should discuss this drug with your health care provider to decide if your symptoms justify the risks. There are many side effects, and because it is an immunosuppressant, it can reduce your ability to fight disease.
Fifth Line: Surgery
Major surgery should be reserved for patients with severe, unresponsive disease, and who are willing to accept the risks and lifelong changes associated with surgery. Surgery can be offered to patients with severely limited bladder capacity or severe symptoms that have not responded to other therapies. Most patients do not require major surgery for this condition. |
Summary |
|
